Mechanistic Rationale: Targeting the "Molecular Glue"
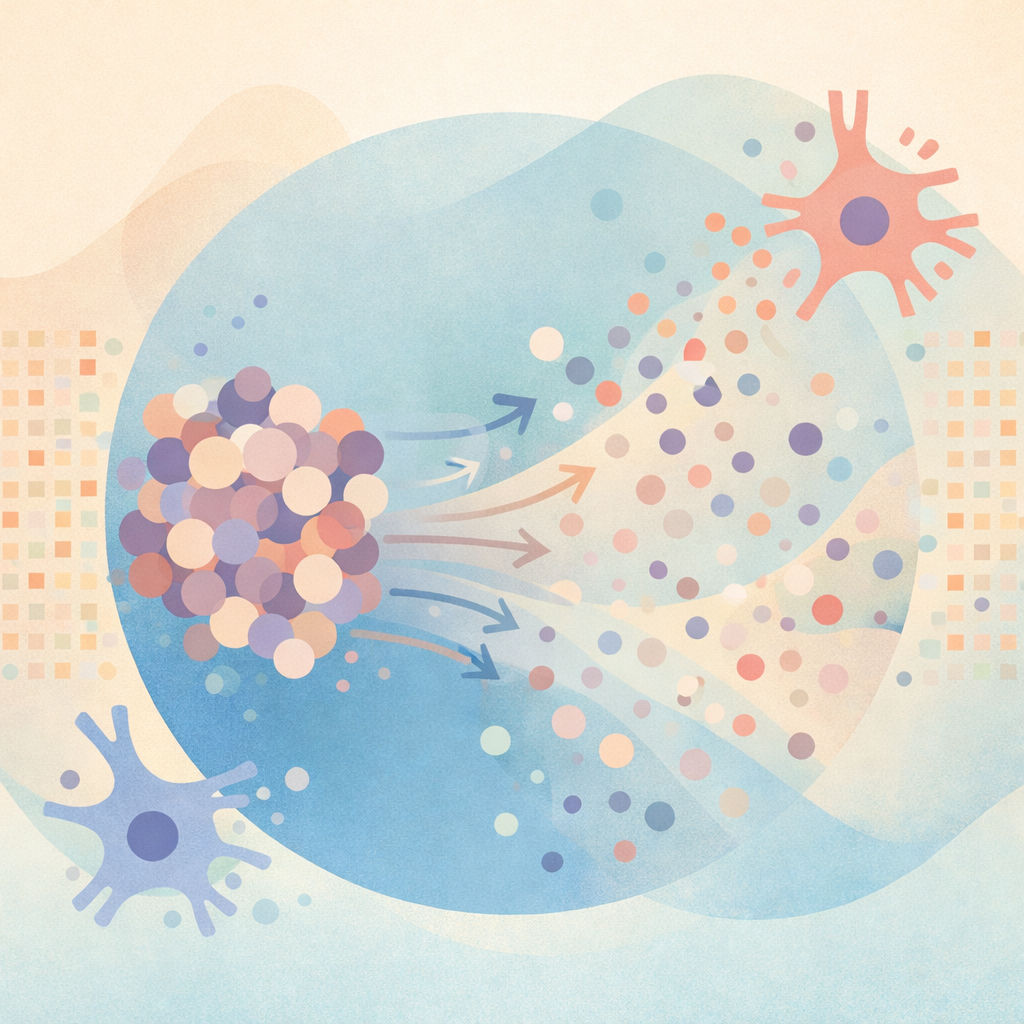
Galectin-3 is overexpressed in activated microglia near amyloid plaques and damaged synapses. It plays a role in AD pathobiology through three mechanisms:
Protein Aggregation (Upstream of Plaque Removal).
Gal-3 acts as a scaffold that facilitates the oligomerization of Aβ, tau, α-synuclein, and APOE4. TB006 binds Gal-3 with high affinity, blocking its scaffolding function, which may prevent new aggregate formation and loosen existing assemblies.Microglial Reprogramming and Neuroinflammation.
Gal-3 serves as an endogenous ligand within TLR-4 and TREM2 signaling, maintaining a pro-inflammatory microglial phenotype. Neutralizing Gal-3 aims to shift microglia to a homeostatic state, thereby reducing cytokine-mediated synaptic toxicity.Liquid-Liquid Phase Separation (LLPS).
Gal-3 contains low-complexity domains that promote LLPS, concentrating misfolded proteins into pathogenic droplets. TB006 is designed to disrupt this concentration effect, reducing aggregation kinetics.
Clinical implication: TB006 functions upstream of amyloid plaque clearance and inflammation, offering a mechanistically distinct approach from approved anti-amyloid antibodies.
Clinical Development and Evidence
Phase 1 and Phase 1b/2a (TB006AD2102)
Population: Mild to severe AD; amyloid status not required.
Design: Seamless dose-escalation followed by proof-of-concept efficacy.
Primary efficacy endpoint (Part 2): Change from baseline in CDR-SB through Day 104.
Key findings (top-line):
CDR-SB: Approximately 63% reduction in clinical decline compared to placebo; p=0.08 (trend, not conventionally significant).
MMSE (secondary): +1.02 points at Day 36 (p=0.02).
Open-Label Extension: After approximately 3 months, 47% showed cognitive improvement ("reversal") and 28% stabilization (uncontrolled data).
Interpretation: These results indicate signal detection, not definitive proof. The short blinded exposure and reliance on secondary endpoints require cautious interpretation.
Safety and Tolerability
ARIA: No ARIA-E/H reported to date, consistent with a non-plaque-stripping mechanism.
Common AEs: Infusion-related reactions.
Dose exposure: Single doses up to 5,000 mg tolerated in healthy volunteers.
Clinical relevance: The apparent ARIA advantage may expand eligibility to patients typically excluded from amyloid-clearing therapies.
Patient Selection and Practical Considerations
Disease stage: Signals observed from mild through severe AD.
Amyloid status: Benefit reported independent of amyloid PET positivity.
Comorbidities: Trials allowed common, treated comorbid conditions.
Expanded Access Program (EAP)
Eligibility: Symptomatic dementia (MMSE <=24), exhausted approved options, trial-ineligible; amyloid PET not required.
Administration: IV infusion (~1 hour) every 28 days.
Cost: Manufacturing-cost recovery (~$5,000 per infusion; ~$20,000 for four months), excluding monitoring/fees.
How TB006 Compares With Anti-Amyloid mAbs
Target: Gal-3 (upstream aggregation/inflammation) vs fibrillar Aβ.
Safety: No ARIA signal reported vs known ARIA risk.
Eligibility: Broader (amyloid-negative; later stages).
Evidence maturity: Early-phase vs FDA-approved agents with registrational trials.
Limitations and Critical Appraisal
Statistical threshold: Primary endpoint missed p<=0.05.
Duration: Short blinded exposure; durability unknown.
Publication status: Much data disseminated via conferences/press releases; peer-reviewed Phase 3 data absent.
Claims of "reversal": Derived from open-label data; require controlled confirmation.
Pipeline Beyond AD
Gal-3 neutralization is being explored in Parkinson's disease (Phase 2a), adult ASD (Phase 2), and glioblastoma (preclinical), reflecting a platform hypothesis centered on aggregation-linked neuroinflammation.
Bottom Line for Clinicians
TB006 introduces a biologically coherent, inflammation-first strategy that may complement or, for selected patients, offer an alternative to amyloid-centric approaches, especially where ARIA risk or amyloid negativity limits options. Enthusiasm should be tempered by the early-phase nature of the evidence. Until registrational trials confirm durability and magnitude of benefit, TB006 is best considered investigational, with EAP use requiring transparent discussion of uncertainty, cost, and goals of care.