Care Management
Our Latest Articles
Early-Stage Caregiving
In early Alzheimer's, individuals stay independent but need help with planning. Care partners are vital in daily tasks, fostering independence, and supporting emotional well-being. They should prioritize self-care and seek support. Understanding Alzheimer's aids in effective care and informed decision-making.
Read moreMemory Domain Impairment: Overview for Patients and Caregivers
Memory involves storing, retaining, and retrieving information, primarily in the hippocampus and assisted by the prefrontal cortex. Impairments range from forgetfulness to disorientation, caused by Alzheimer's, vascular dementia, TBI, and substance abuse. Early recognition and support enhance quality of life.
Read moreExecutive Function Domain: A Guide for Patients and Caregivers
Executive function, crucial for managing thoughts, actions, and emotions, is mainly localized in the prefrontal cortex. Impairment affects decision-making and behavior, caused by dementia, brain injury, or mental health issues. Management includes therapy, support groups, memory aids, routines, apps, and healthy practices.
Read moreVisuospatial Skills Domain: A Guide for Patients and Caregivers
Visuospatial skills enable spatial understanding and object visualization, primarily in the right parietal lobe. Impairments, due to conditions like Alzheimer's or stroke, affect tasks such as navigation and object recognition. Management strategies include therapy, environmental changes, adaptive tools, and support for independence.
Read moreLanguage Domain: A Guide for Patients and Caregivers
The language domain involves the brain's ability to process communication, primarily in the left hemisphere. Impairments, such as aphasia, can affect quality of life and are caused by conditions like stroke and Alzheimer's. Management includes speech therapy, AAC, and support to help maintain communication abilities.
Read moreAttention/Concentration Domain: A Guide for Patients and Caregivers
The attention and concentration domain involves brain areas like the frontal and parietal lobes, thalamus, and anterior cingulate cortex. Impairments can stem from ADHD, dementia, TBI, and depression. Management strategies include CBT, mindfulness, routines, and apps. Consulting healthcare providers for personalized strategies is advised.
Read moreSocial/Emotional Domain: A Guide for Patients and Caregivers
The social, emotional, and behavioral domain involves brain areas such as the prefrontal cortex and amygdala, influencing empathy and impulse control. Conditions like ASD and TBI can impair these functions. Therapy, social skills training, mindfulness, and caregiver support can help manage symptoms
Read moreMotor/Sensory Domain: A Guide for Patients and Caregivers
The motor and sensory domain involves movement and sensation, controlled by the motor cortex, somatosensory cortex, cerebellum, and basal ganglia. Impairments from conditions like Parkinson's, stroke, and MS affect coordination and sensory processing. Management includes therapy, assistive devices, and caregiver support.
Read moreUnderstanding the Progression of Dementia
Families often compare dementia to reverse aging. Individuals first lose complex skills like managing finances or work duties. Over time, they struggle with everyday tasks such as cooking and dressing, eventually requiring help with basic self-care.
Read moreUnderstanding Different Types of Alzheimer's Disease
Alzheimer's disease includes forms like PCA (visual processing), lvPPA (language), CBS (movement/cognition), Amnestic (memory), and Executive (executive functions). Diagnosis involves cognitive tests, imaging, and neurological exams to create tailored care plans, aiding effective symptom management.
Read moreUnderstanding Different Types of Frontotemporal Disease
Frontotemporal lobar degeneration (FTLD) includes neurodegenerative disorders affecting the frontal and temporal brain lobes, impacting behavior, language, and motor functions. Types include bvFTD, svPPA, nfvPPA, PSP, and CBS. Diagnosis involves neuropsychological tests, brain imaging, and neurological exams.
Read moreUnderstanding Different Types of Alpha-synuclein Disease
Synucleinopathies, including Parkinson's Disease, Dementia with Lewy Bodies, Parkinson's Disease Dementia, Multiple System Atrophy, and REM Sleep Behavior Disorder, are neurological disorders caused by abnormal alpha-synuclein in the brain, affecting movement, cognition, and sleep. Diagnosis uses exams, imaging, and studies to guide care.
Read moreWhat is Mild Cognitive Impairment?
Understanding cognitive decline, from subjective cognitive impairment (SCI) to mild cognitive impairment (MCI) and dementia, is crucial as the population ages. SCI involves self-reported changes, MCI shows measurable deficits, and dementia severely impacts daily life. Biomarkers aid diagnosis, but early detection and research are vital for better outcomes.
Read moreWhat is Beta-Amyloid?
Alzheimer's disease is characterized by beta-amyloid protein accumulation, particularly A42, which obstructs the glymphatic system and causes neurodegeneration. Low A42 and high tau proteins in cerebrospinal fluid serve as diagnostic markers. Early diagnosis enables treatments to slow disease progression.
Read moreWhat is Lecanemab
The text highlights a shift in Alzheimer's treatment to disease-modifying therapies, focusing on FDA-approved lecanemab. It targets amyloid plaques, potentially slowing progression by 30% if started early. Side effects are manageable, and personal risk assessments suggest it as a hopeful option for early intervention.
Read moreThe MIND Diet and Brain Health
The MIND diet, developed in 2015, combines elements of the Mediterranean and DASH diets to boost brain health. It focuses on leafy greens and whole grains while reducing red meat and sweets. Although initial studies showed positive associations, recent trials found no significant effects, prompting
Read morePhysical Exercise and Brain Health
As the global population ages, dementia prevalence increases, posing public health challenges. Physical activity may reduce dementia risk by enhancing cognitive reserve, protecting cerebrovascular health, and reducing amyloid-. Guidelines recommend 150 minutes of moderate exercise weekly. Further research is needed.
Read moreSleep and Brain Health
Sleep is crucial for brain health, influencing cognition and memory, and helping prevent cognitive decline. Managing sleep issues can involve non-drug methods like sleep hygiene and CBT-I, as well as medications like DORAs. Personalized strategies developed with healthcare professionals are important.
Read moreUnderstanding APOE: Genetic Blueprint for Brain and Heart Health
The APOE gene, with variants 2, 3, and 4, affects fat processing and brain health. APOE-4 increases Alzheimer's and heart disease risk, but lifestyle choices like diet, exercise, and stress management can mitigate this. A diet rich in leafy greens, berries, nuts, and fatty fish, along with regular health monitoring, can help reduce risks associated with APOE-4.
Read moreYour Guide to Understanding Neurocognitive Test Results
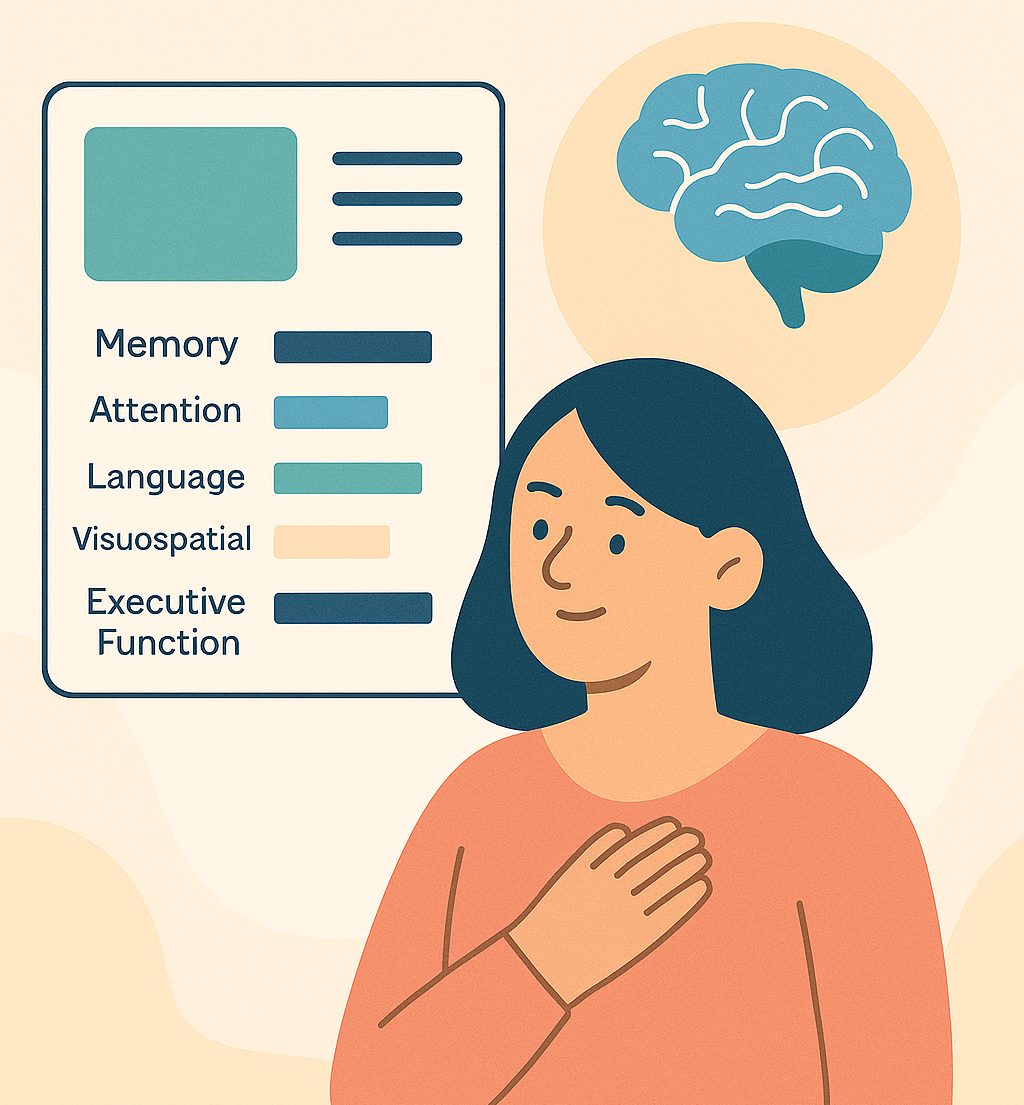
The neurocognitive report evaluates brain functions such as memory, attention, language, visuospatial skills, and executive function, comparing them to age and background norms. Scores indicate if you are average, below, or above average, but patterns matter more than single scores. Discuss results with a healthcare provider, monitor changes over time, and maintain healthy habits to support brain health. Stress, mood, and lifestyle can affect scores, and low scores don't necessarily indicate dementia.
Read moreYour Brain on Estrogen: How Hormones, Lifestyle, and Smart Choices Protect Your Mind for Life
Women's brain health deserves special attention as they face unique challenges during menopause when estrogen levels decline, impacting brain energy and function. Estrogen is crucial for memory and mood regulation. Lifestyle changes, such as diet and exercise, can help maintain brain health. Hormone therapy may aid menopause symptoms but does not prevent Alzheimer's. Women in midlife should prioritize brain health, considering personal risks and exploring options with healthcare providers.
Read moreNAD: From Cellular Metabolism to Neuroprotection
Over the past 30 years, nicotinamide adenine dinucleotide (NAD+) has transformed from a little-known biochemical substrate in dehydrogenase reactions to a crucial focus in aging, neurodegeneration, and cellular resilience research. Initially a metabolic curiosity linked to vitamins, NAD+ now stands
Read moreA New Way Forward: The Subcutaneous Version of Lecanemab (LEQEMBI)
A New Way Forward: The Subcutaneous Version of Lecanemab (LEQEMBI) By James F. Rini, MDThe treatment landscape for early Alzheimer's disease is changing rapidly. We are advancing from symptom management to therapies that target the disease itself. Lecanemab, now available in a subcutaneous form,
Read moreUnderstanding Dementia
This article provides a clear narrative, focusing on patients and caregivers. It explores each concept in depth, aligning with modern neurocognitive best practices. The language is accessible and informative, ensuring clarity and engagement for all readers.
Read moreThe Four Foundations of Neurolongevity
Neurolongevity focuses on maintaining brain function, independence, and quality of life, rather than preventing aging or eliminating disease. It aims to preserve cognitive abilities for as long as possible, even when faced with medical conditions or neurodegenerative challenges.
Read more