Understanding Parkinson's Disease
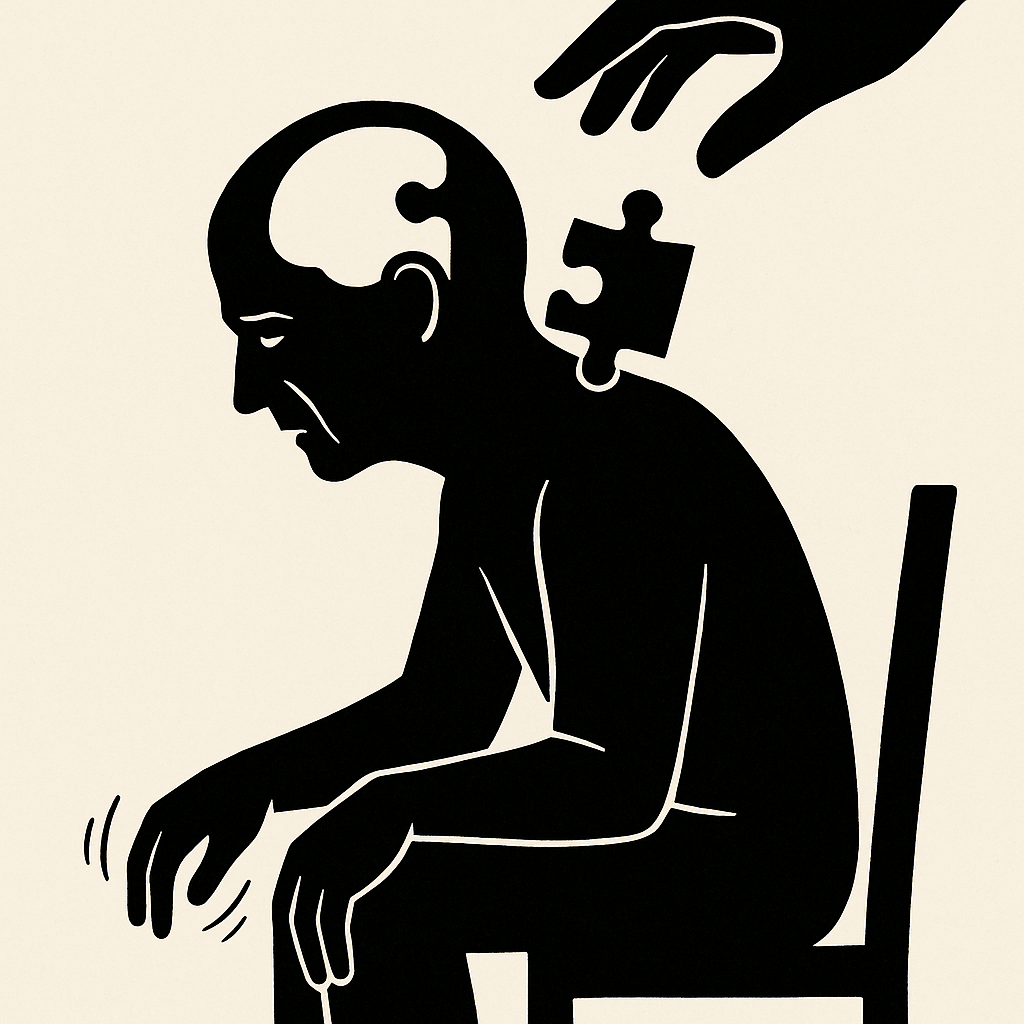
Parkinson's disease, the second most common neurodegenerative disorder, continues to present significant diagnostic challenges, particularly in its early and prodromal stages. Increasingly, the condition is understood as more than a motor disorder, with a wide spectrum of non-motor features and genetic underpinnings reshaping the way clinicians classify and approach the disease.
Diagnostic Challenges and Non-Motor Symptoms
Traditionally, diagnosis has relied on the hallmark motor symptoms of bradykinesia, rigidity, and tremor. Yet many patients first exhibit non-motor manifestations, including hyposmia, sleep disturbances, and autonomic dysfunction, which often precede motor onset by years. These prodromal symptoms represent a critical diagnostic window. Recognizing and validating them with objective markers could enable earlier identification and timely intervention.
Heterogeneity and Personalized Treatment
Another key theme is heterogeneity. Parkinson's disease is not a uniform entity but rather a spectrum of subtypes with different trajectories and treatment responses. Recent cluster analyses that integrate non-motor as well as motor features have helped to delineate clinically meaningful subgroups. For instance, the "diffuse malignant" subtype - marked by mild cognitive impairment, REM sleep behavior disorder, and orthostatic hypotension - progresses rapidly and demands distinct therapeutic considerations. Such classification underscores the need for a personalized approach to treatment.
The Role of Genetics
Genetics is increasingly central to this shift. Mutations in genes such as LRRK2, PARK7, PINK1, and SNCA have been implicated in familial parkinsonism, while genome-wide association studies have uncovered numerous loci contributing to sporadic disease. Genetic testing, particularly in early-onset cases or those with family history, is moving into mainstream practice. Beyond diagnosis, these discoveries are paving the way for targeted therapies tailored to underlying molecular pathways.
Advancements in Biomarkers
Diagnostic practice is also being reshaped by biomarkers. Although olfactory testing and conventional structural MRI currently serve as adjuncts, advances in imaging - such as neuromelanin-sensitive MRI and quantitative susceptibility mapping - are opening new possibilities. At the molecular level, cerebrospinal fluid and peripheral tissue markers of alpha-synuclein pathology are emerging as powerful tools. Together, these developments promise earlier, more accurate detection, potentially even in preclinical stages, where neuroprotective strategies might have their greatest impact.
A New Era of Diagnosis and Treatment
The field is entering a new era: one where diagnosis evolves from clinical acumen alone to a biomarker-supported, subtype-informed process. This transformation not only enables earlier identification but also opens pathways to precision medicine, with therapeutic strategies tailored to the biological and clinical profile of each patient. Ultimately, such progress holds the promise of improving prognosis, slowing disease progression, and enhancing quality of life for those affected by Parkinson's disease.