A Guide for Patients and Caregivers
If you or someone you care for has been diagnosed with early Alzheimer's disease, you may have heard about new treatments often referred to as anti-amyloid therapies. These medications represent a significant scientific milestone, but they can also be confusing, overwhelming, and emotionally charged.
This article aims to help you understand what these treatments are, how they were developed, what they may (and may not) do, what risks they carry, and how to consider if they are right for you or your family.
There is no single "right" choice. The goal is understanding - not pressure.
A Brief History: Why These Treatments Exist
For decades, Alzheimer's disease treatment focused mainly on symptoms, not the underlying disease. Medications such as donepezil or memantine can help with thinking, attention, or daily function for some people, but they do not change the biology of Alzheimer's disease.
Researchers have long known that Alzheimer's disease is associated with an abnormal buildup of a protein called amyloid beta, which forms plaques in the brain years before symptoms appear. These plaques are believed to trigger a cascade of injury involving other proteins (such as tau), inflammation, and gradual loss of brain cells.
After many unsuccessful attempts, scientists developed laboratory-engineered antibodies that could recognize and attach to amyloid beta and assist the body in removing it from the brain.
This led to the development of two medications now fully approved by the U.S. Food and Drug Administration:
- Lecanemab (approved in 2023)
- Donanemab (approved in 2024)
These are the first treatments shown to modify the course of Alzheimer's disease itself, rather than only treating symptoms.
What Are Anti-Amyloid Therapies?
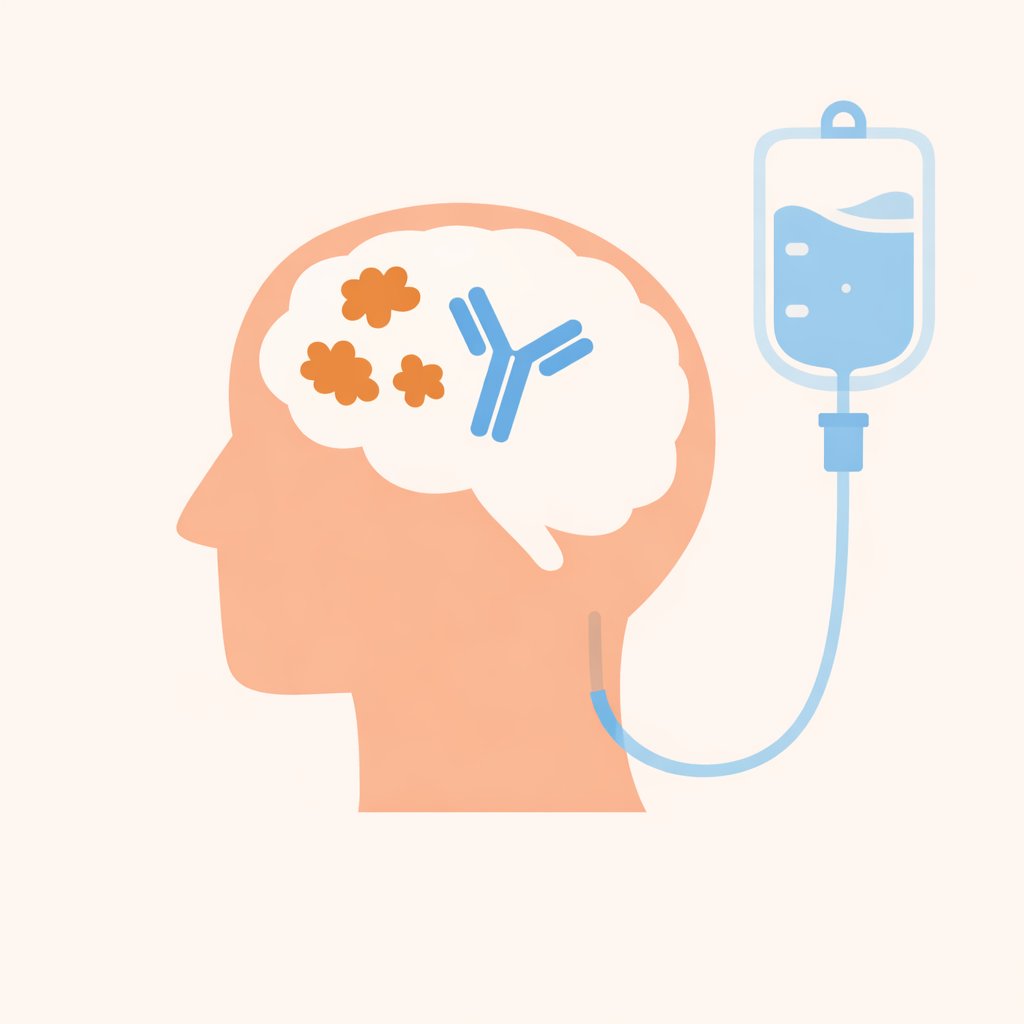
Anti-amyloid therapies are monoclonal antibodies - specialized proteins designed to recognize a specific target. In this case, the target is amyloid beta. Once the antibody attaches to amyloid, it signals the brain's immune system to help clear amyloid deposits over time.
Important points:
- These medications are given by intravenous infusion (through a vein).
- They are not pills.
- They are long-term treatments, typically over many months.
How Do These Medications Work in the Brain?
Think of amyloid plaques like debris accumulating in a river. Anti-amyloid antibodies:
- Attach to amyloid
- Mark it for removal
- Allow the brain's cleanup systems to gradually reduce plaque burden
This process:
- Happens slowly
- Requires ongoing treatment
- Does not repair damage already done
Clearing amyloid appears to slow further injury, but it does not restore lost brain cells or memories.
Who Are These Treatments For?
Anti-amyloid therapy is intended only for people in the earliest stages of Alzheimer's disease, including:
- Mild cognitive impairment (MCI) due to Alzheimer's disease
- Very mild dementia due to Alzheimer's disease
Before treatment, doctors must confirm that amyloid is actually present in the brain, using:
- An amyloid PET scan or
- A spinal fluid (lumbar puncture) test
These treatments are not appropriate for:
- Moderate or advanced Alzheimer's disease
- Other causes of memory loss (such as Lewy body dementia, frontotemporal dementia, vascular dementia, Parkinson's disease, or stroke-related cognitive impairment)
What Benefits Can These Medications Provide?
This is the most important - and most misunderstood - question.
What Studies Show
In carefully selected patients with early Alzheimer's disease, these medications:
- Reduce amyloid plaques in the brain
- Slow cognitive and functional decline modestly
On average, this slowing translates into months of delayed progression, not years, and not recovery.
What This Means in Real Life
These treatments may help some people stay at a milder stage longer, preserving:
- Independence
- Daily functioning
- Sense of self
They do not:
- Cure Alzheimer's disease
- Restore lost memories
- Stop the disease completely
Many people find it helpful to think of anti-amyloid therapy as buying time, rather than changing the destination.
What Are the Risks?
All medications have risks. Anti-amyloid therapies have some unique and serious considerations.
ARIA: Brain Swelling or Bleeding
The most important risk is something called ARIA (Amyloid-Related Imaging Abnormalities), which can involve:
- Brain swelling
- Small areas of bleeding in the brain
Most cases are mild and detected on MRI before symptoms appear, but some people may experience:
- Headache
- Confusion
- Dizziness
- Vision changes
- Nausea
- Difficulty walking
- Seizures (rare)
Very rarely, ARIA can be severe or life-threatening.
Who Is at Higher Risk?
Risk is higher in:
- People with certain genetic traits (APOE-e4)
- People on blood-thinning medications
- People with certain MRI abnormalities
Because of this risk, regular MRI scans are required during treatment.
How Intensive Is Treatment?
Anti-amyloid therapy is not just a medication - it is a care pathway.
Treatment typically involves:
- Regular infusions (every 2-4 weeks)
- Scheduled MRI scans
- Frequent clinic visits
- Ongoing monitoring for symptoms
- A caregiver or support person who can help watch for changes
Many families decide whether to proceed based on whether this level of medical involvement fits realistically into their lives.
What Happens if Treatment Has to Stop?
Stopping treatment:
- Is not dangerous
- Is not a failure
- Does not worsen the disease beyond its natural course
Treatment may be paused or stopped if:
- Side effects occur
- MRI changes appear
- The burden outweighs the benefit
- Personal goals change
These decisions are part of good medical care.
Can Other Alzheimer's Medications Be Continued?
Yes. Medications such as donepezil, rivastigmine, galantamine, or memantine can usually be continued alongside anti-amyloid therapy.
Anti-amyloid treatment does not replace:
- Symptom-based medications
- Lifestyle interventions
- Cognitive support
- Emotional and caregiver support
What About Cost and Insurance?
Coverage varies by insurance plan. While Medicare covers these medications, patients may still face:
- Copays
- MRI costs
- Infusion-related charges
- Travel and time costs
Your care team should help you understand potential financial responsibilities before treatment begins.
How Should Patients and Caregivers Think About This Decision?
This is not just a medical decision - it is a values decision.
Helpful questions to consider:
- How do we define "quality of life" right now?
- Is slowing decline worth frequent medical visits and monitoring?
- How do we feel about risk versus potential benefit?
- What matters most to us in this stage of life?
Choosing yes or no can both be thoughtful, informed, and compassionate decisions.
A Final Word
Anti-amyloid therapies represent meaningful scientific progress, but they are not a cure. They offer the possibility of slowing Alzheimer's disease in some people - at the cost of medical intensity, uncertainty, and risk.
The most important part of this process is not the medication itself, but shared decision-making - honest conversations between patients, caregivers, and clinicians about goals, values, and expectations.
You deserve time, clarity, and support in making this choice.
If you have questions, bring them to your care team. No question is too small, and no decision needs to be rushed.