Frontotemporal lobar degeneration (FTLD) encompasses a diverse spectrum of progressive neurodegenerative disorders characterized by language, behavior, and motor impairments. The two most common pathological subtypes are FTLD with tau protein inclusions (FTLD tau) and FTLD with TAR DNA binding protein of 43 kDa (FTLD TDP). Differentiating between these subtypes during life remains a critical challenge in clinical practice due to the extensive overlap in clinical symptoms and the lack of reliable in vivo biomarkers. Currently, definitive diagnosis requires postmortem neuropathological examination, limiting the ability to accurately stratify patients for targeted therapeutic interventions.
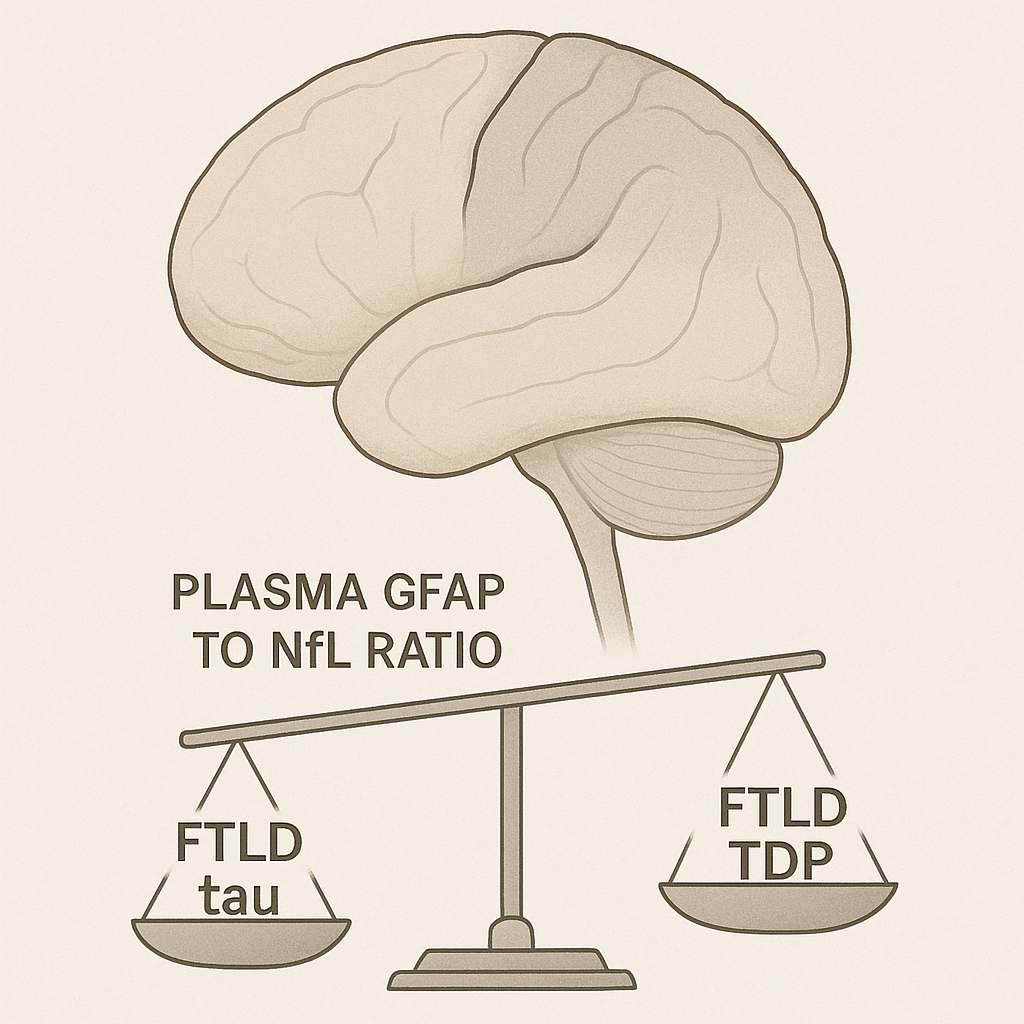
Recent work by Cousins and colleagues has provided compelling evidence that the plasma ratio of glial fibrillary acidic protein (GFAP) to neurofilament light chain (NfL) can serve as a promising biomarker to distinguish FTLD tau from FTLD TDP in living patients. This discovery holds significant clinical implications for improving diagnostic precision and expanding access to disease-modifying clinical trials.
Study Overview
The investigation was conducted as a retrospective cross-sectional study using data collected between 2009 and 2020 from the University of Pennsylvania Integrated Neurodegenerative Disease Database. The study analyzed plasma biomarkers in two major cohorts:
- Training Sample: Included 141 patients with autopsy-confirmed and/or genetically confirmed FTLD tau (n = 46) and FTLD TDP (n = 95). Thirty-one cognitively unimpaired controls were also included. Pathological confirmation relied on expert neuropathological examination or detection of pathogenic variants such as MAPT for FTLD tau and C9orf72, GRN, or TARDBP for FTLD TDP.
- Validation Sample: Consisted of 62 patients with clinical diagnoses predictive of underlying pathology, including progressive supranuclear palsy syndrome associated with tau (PSPS tau, n = 31) and amyotrophic lateral sclerosis associated with TDP-43 (ALS TDP, n = 31).
Plasma GFAP and NfL levels were quantified using the Quanterix single molecule array (Simoa) platform. For patients lacking autopsy data, cerebrospinal fluid amyloid beta 42 or the amyloid beta 42 to 40 ratio was used to exclude coexisting Alzheimer pathology.
Key Findings
Superiority of the GFAP to NfL Ratio
- The plasma GFAP to NfL ratio demonstrated excellent ability to discriminate between FTLD tau and FTLD TDP.
- In the autopsy-confirmed training sample, the ratio achieved an area under the receiver operating characteristic curve (AUC) of 0.89, with a sensitivity of 0.73 and specificity of 0.89.
- When the threshold of 2.73 was applied to the independent validation sample, sensitivity was 0.84 and specificity was 0.81.
- This performance exceeded that of either GFAP alone (AUC 0.65) or NfL alone (AUC 0.75).
Patterns of Individual Biomarkers
- GFAP levels were generally higher in FTLD tau, consistent with astrogliosis as a prominent feature in tauopathies. NfL levels were significantly higher in FTLD TDP, reflecting more extensive axonal degeneration associated with this pathology. Importantly, NfL correlated positively with the burden of TDP-43 pathology, whereas the GFAP to NfL ratio correlated positively with tau burden and inversely with TDP-43 burden.
Consistency Across Clinical and Pathological Subtypes
- The GFAP to NfL ratio performed consistently across various pathological and clinical subtypes, including sporadic behavioral variant FTD and primary progressive aphasia. Even when variant carriers were excluded, diagnostic accuracy remained high. This finding underscores the robustness of the ratio, particularly for sporadic FTLD cases that are otherwise difficult to classify.
Clinical Implications
Antemortem Diagnosis
- The GFAP to NfL ratio provides a minimally invasive plasma-based tool to distinguish between FTLD tau and FTLD TDP during life. This capability addresses a critical unmet need in diagnosing sporadic FTLD, where current clinical assessments and imaging often fall short of identifying underlying pathology.
Patient Selection for Clinical Trials
- Disease-modifying therapies targeting specific proteinopathies require accurate patient selection. The ability to identify the correct pathological subtype in sporadic cases could allow inclusion of these patients in clinical trials, thereby accelerating therapeutic development.
Understanding Disease Mechanisms
- The distinct biomarker signatures observed for GFAP and NfL levels highlight underlying differences in neuroinflammatory and neurodegenerative mechanisms between FTLD tau and FTLD TDP. This knowledge may guide future therapeutic strategies.
Considerations for Clinical Practice
While the GFAP to NfL ratio holds promise, several factors must be considered in its clinical application:
- Genetic Testing: Genetic status influences biomarker interpretation. Many false positive results for FTLD TDP were associated with variant carriers.
- Disease Stage: Plasma biomarker levels vary with disease duration and severity. A single universal threshold may not apply across all disease stages.
- Alzheimer Pathology: Given the clinical overlap between FTD and Alzheimer disease, a two-step diagnostic algorithm that first excludes Alzheimer pathology may be necessary.
- Population Diversity: The study sample was predominantly White, necessitating further validation in more diverse populations.
Conclusion
The plasma GFAP to NfL ratio emerges as a promising biomarker for distinguishing FTLD tau from FTLD TDP during life. Its high diagnostic accuracy, robustness across clinical phenotypes, and potential to expand patient eligibility for targeted interventions make it a valuable tool in clinical and research settings. Further longitudinal and multicenter studies are warranted to validate its use across broader populations and disease stages.