The search for reliable biomarkers for neurodegenerative diseases has led to growing interest in skin alpha-synuclein as a diagnostic and prognostic tool for synucleinopathies. These disorders, including Parkinson's disease (PD), dementia with Lewy bodies (DLB), multiple system atrophy (MSA), and pure autonomic failure (PAF), are characterized by the aggregation of alpha-synuclein, a protein implicated in their pathophysiology. Emerging evidence supports the use of skin alpha-synuclein detection as a minimally invasive and accessible biomarker for these conditions. Below, we provide an overview of the key findings and their clinical implications for physicians.
The Role of Alpha-Synuclein in Synucleinopathies
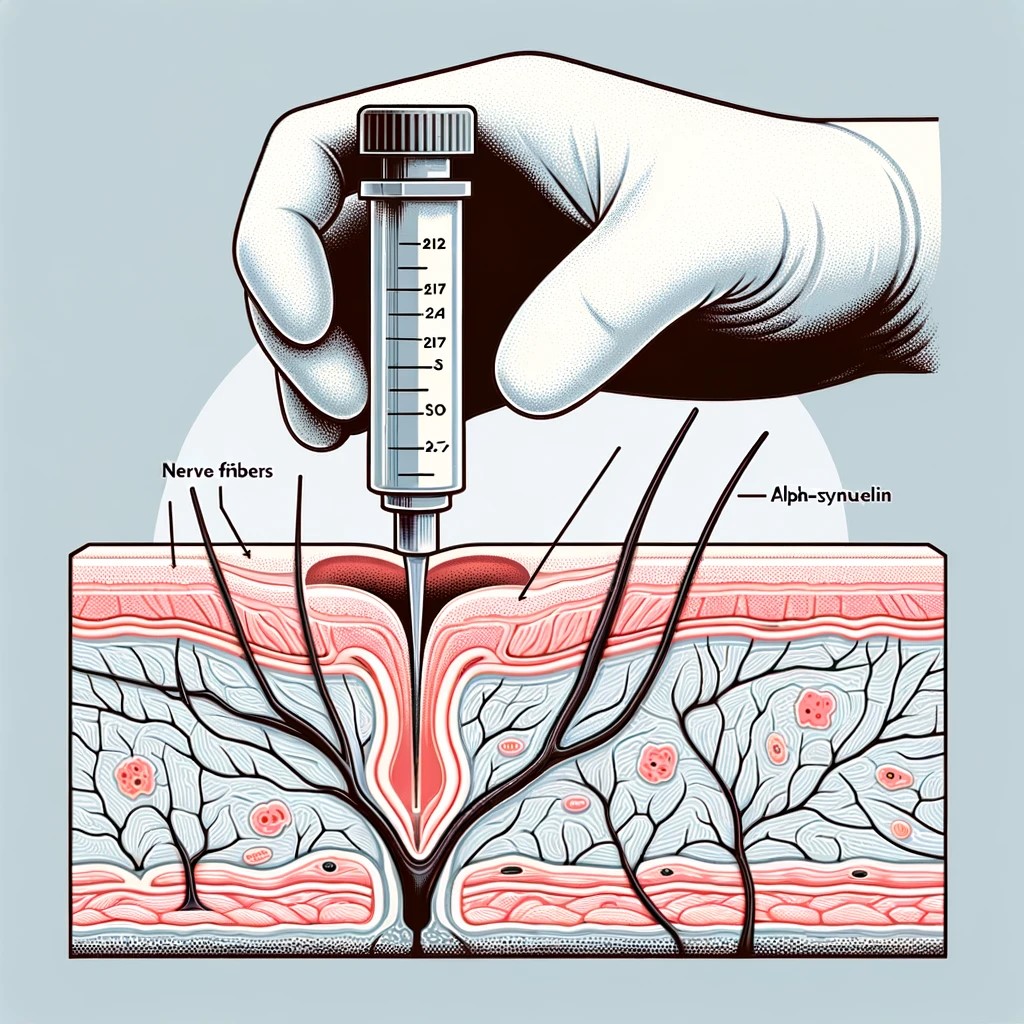
Alpha-synuclein, a protein primarily located at presynaptic terminals in the brain, plays a role in synaptic vesicle trafficking and neurotransmitter release. However, under pathological conditions, it misfolds and aggregates into toxic forms such as Lewy bodies and neurites, which are the hallmark pathological features of synucleinopathies. While traditionally associated with the central nervous system, alpha-synuclein aggregates have also been identified in the peripheral nervous system, including in cutaneous nerve fibers. This finding has opened the door for skin-based diagnostic approaches.
Key Findings from Medical Literature
- Presence of Alpha-Synuclein in Skin Nerves:
- Alpha-synuclein deposits are detectable in skin nerve fibers, offering a peripheral biomarker for diseases primarily associated with brain pathology. These deposits reflect the systemic nature of synucleinopathies, which extend beyond the central nervous system.
- Phosphorylated Alpha-Synuclein (p-syn) as a Pathological Marker:
- While alpha-synuclein exists in healthy tissue, its phosphorylated form (p-syn) is predominantly associated with pathological states. Detecting p-syn in skin biopsies enhances diagnostic specificity for synucleinopathies.
- Diagnostic Accuracy:
- Multiples studies have demonstrated the diagnostic utility of skin biopsies. The sensitivity and specificity of skin biopsies is still being explored but in general is very promising:
- PD: 92.7% sensitivity for detecting p-syn.
- MSA: 98.2% sensitivity.
- DLB: 96.0% sensitivity.
- PAF: 100% sensitivity.
- These results highlight the potential of skin biopsies as a valuable diagnostic tool for differentiating these conditions.
- Multiples studies have demonstrated the diagnostic utility of skin biopsies. The sensitivity and specificity of skin biopsies is still being explored but in general is very promising:
- Distinguishing Between Synucleinopathies:
- The distribution pattern of p-syn in skin nerves differs between synucleinopathies:
- In PD, p-syn is primarily observed in autonomic fibers innervating sweat glands and arrector pili muscles.
- In MSA, p-syn deposits are predominantly found in unmyelinated somatosensory fibers. These patterns can aid in differentiating between these clinically overlapping conditions.
- The distribution pattern of p-syn in skin nerves differs between synucleinopathies:
- Advantages of Skin Biopsy:
- Minimally Invasive: Compared to brain biopsies or lumbar punctures, skin biopsies are safer and more patient-friendly.
- Repeatable: They can be performed repeatedly, enabling longitudinal monitoring of alpha-synuclein deposition.
- Cost-Effective: Skin biopsies are generally less expensive than advanced imaging techniques.
Challenges and Areas for Future Research
While the findings are promising, several challenges need to be addressed before skin alpha-synuclein can be widely adopted in clinical practice:
- Standardization of Protocols:
Variations in biopsy techniques, tissue processing, and staining methods have resulted in inconsistencies across studies. Establishing standardized protocols is essential for ensuring reliability and comparability of results. - Larger, Diverse Studies:
Current studies often involve small, homogenous cohorts. Larger-scale research involving diverse populations is necessary to validate findings and assess the biomarker's accuracy across different ethnic and genetic backgrounds. - Correlation with Disease Progression:
The relationship between skin alpha-synuclein levels and disease progression remains unclear. Future studies should explore whether changes in alpha-synuclein deposition over time correlate with clinical symptoms and disease severity, providing prognostic insights. - Seed Amplification Assays (SAA):
SAA techniques have recently shown promise in detecting alpha-synuclein aggregation activity in skin samples. These assays could further enhance sensitivity and may complement traditional methods.
Clinical Implications for Physicians
The integration of skin alpha-synuclein testing into clinical workflows has several potential benefits:
- Early Diagnosis: Detecting p-syn in skin biopsies may facilitate earlier diagnosis of synucleinopathies, enabling timely interventions.
- Differentiation of Disorders: The ability to distinguish between PD, MSA, and other synucleinopathies through skin biopsy could improve diagnostic accuracy, reducing misdiagnoses.
- Longitudinal Monitoring: Repeatable skin biopsies provide a practical option for tracking disease progression and evaluating treatment response.
For physicians managing patients with suspected synucleinopathies, skin biopsies represent an exciting diagnostic tool with broad implications for improving patient outcomes.
Conclusion
Skin alpha-synuclein offers a minimally invasive, safe, and repeatable biomarker for the diagnosis and monitoring of synucleinopathies. While further research is needed to standardize protocols and validate findings in larger populations, the current evidence underscores its potential to revolutionize the clinical approach to these disorders. By incorporating skin alpha-synuclein testing into routine practice, physicians may enhance diagnostic accuracy, facilitate earlier interventions, and improve the overall management of patients with neurodegenerative diseases.

