In a landmark cross-sectional study recently published in JAMA Neurology (April 2025), Skillback et al. examined cerebrospinal fluid (CSF) biomarkers in over 13,800 individuals diagnosed with dementia in Sweden. This research provides critical insights into the distribution and prognostic value of Alzheimer's-related pathology beyond clinical Alzheimer's disease (AD).
Study Design and Cohort Characteristics
This 12-year registry-based study combined clinical records from the Swedish Dementia Registry (SveDem) with routine CSF biomarker analyses conducted at Sahlgrenska University Hospital. The cohort included patients with a confirmed dementia diagnosis and complete CSF profiles (Aβ1-42, total tau [t-tau], and phosphorylated tau [p-tau181]) measured within three years of diagnosis. Diagnoses included Alzheimer variants (early- and late-onset), vascular dementia (VAD), mixed dementia (AD/VAD), frontotemporal dementia (FTD), dementia with Lewy bodies (DLB), Parkinson disease dementia (PDD), and dementia not otherwise specified (NOS).
Biomarker Profiles and Diagnostic Discrimination
Patients with early-onset AD had the most pronounced biomarker changes: significantly lower CSF Aβ1-42, higher t-tau and p-tau, and reduced Aβ1-42/p-tau ratios. Similar patterns were observed in late-onset AD and mixed dementia, though with slightly less pronounced deviations. Importantly, 84% of early-onset AD, 81% of late-onset AD, and 76% of mixed dementia patients exhibited pathological Aβ1-42 concentrations.
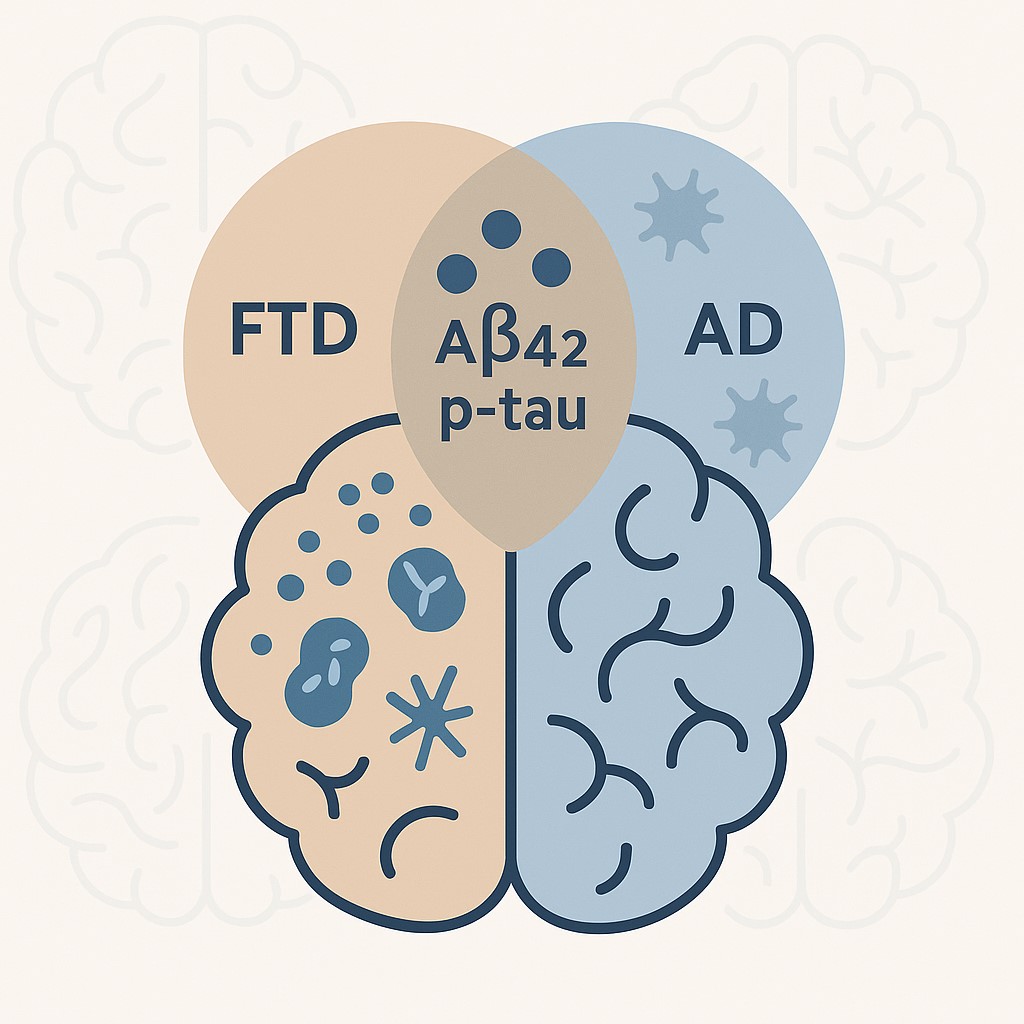
Notably, a significant minority of patients with non-AD diagnoses also demonstrated AD-like biomarker profiles. DLB showed 59% Aβ positivity, while 27% of FTD patients and 16% of those with PDD exhibited elevated tau markers, challenging the notion of purely segregated pathological phenotypes.
The dementia NOS group had the highest percentage of patients with complete AD biomarker triads (25%) among non-AD diagnoses, suggesting either diagnostic uncertainty or high rates of co-pathology. FTD and PDD had the lowest rates of triad positivity (8% and 9%, respectively).
Cognitive Correlates and Diagnostic Implications
MMSE scores were modestly but significantly associated with biomarker abnormalities, particularly CSF Aβ1-42 and the Aβ1-42/p-tau ratio, in AD and some non-AD groups (e.g., VAD, FTD). Interestingly, p-tau181 concentrations were not independently predictive of MMSE across any diagnostic category, limiting its utility as a direct correlate of global cognitive function.
These findings highlight the nuanced relationship between biomarker expression and clinical phenotype. While AD biomarkers align with cognitive impairment in classical AD, their presence in non-AD dementias may reflect co-pathology or early-stage comorbidity, emphasizing the necessity for longitudinal biomarker surveillance.
Sex, Setting, and Diagnostic Context
Sex differences emerged: women had higher p-tau and t-tau concentrations in several groups (including AD and DLB), while men exhibited higher Aβ1-42/p-tau ratios in late-onset AD. Specialist care settings were more likely to diagnose cases after CSF analysis (88% of cases), suggesting a growing reliance on biomarker data in clinical decision-making. Notably, biomarker patterns differed based on whether diagnoses were made before or after lumbar puncture, highlighting potential circularity in biomarker-informed diagnoses.
Clinical Implications and Future Directions
This study provides robust population-level evidence that AD biomarker signatures are not exclusive to clinical AD. In the setting of symptomatic dementia, the presence of Aβ and tau abnormalities may indicate true co-pathology rather than misdiagnosis, especially in mixed or ambiguous presentations such as DLB or dementia NOS. Given the advent of anti-amyloid therapies, such as lecanemab and donanemab, these findings are highly relevant to therapeutic selection and monitoring.
However, the study also reminds clinicians to interpret CSF findings within the broader clinical context, especially in non-AD dementias where MMSE may inadequately capture disease burden, and where CSF positivity may represent secondary, not primary, pathology.
Conclusion
CSF biomarkers of AD, namely Aβ1-42, t-tau, and p-tau181, are powerful diagnostic tools with relevance extending beyond Alzheimer's disease. Their integration into routine diagnostic algorithms should be guided by both clinical phenotype and recognition of co-pathologic patterns. As disease-modifying therapies become more widely available, a refined biomarker-guided approach to dementia subtyping will be essential for individualized care.
Citation:
Skillback, T., Jonsson, L., Skoog, I., et al. (2025). Cerebrospinal Fluid Biomarkers for Alzheimer Disease Among Patients With Dementia. JAMA Neurology. Published online April 28, 2025. https://doi.org/10.1001/jamaneurol.2025.0693