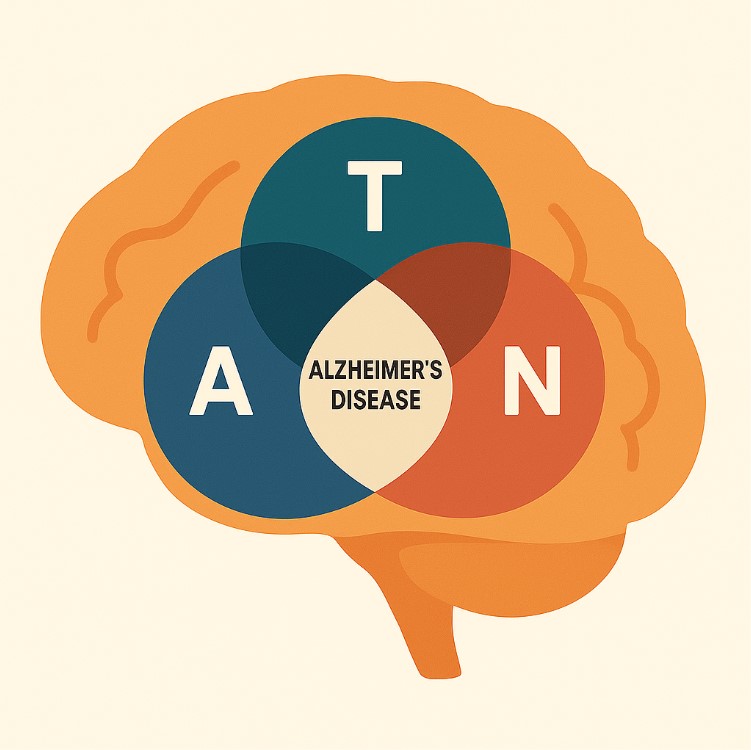
As Alzheimer's disease (AD) research shifts from symptom management to early detection and prevention, biomarkers have become essential in understanding and tracking the disease's progression. In 2016, Clifford R. Jack Jr. and colleagues introduced the A/T/N framework, a biological classification system to categorize individuals based on the presence of core AD-related pathologies. This framework provides a clear, unbiased, and inclusive approach to describing disease biology across the cognitive aging spectrum, regardless of clinical symptoms.
What Is the A/T/N Framework?
The A/T/N system organizes seven established AD biomarkers into three binary categories:
- A (Amyloid pathology):
- Measured via amyloid PET or CSF Aβ42 levels.
- A positive (A+) result indicates the presence of β-amyloid plaques, a hallmark of AD.
- T (Tau pathology):
- Measured through CSF phosphorylated tau (p-tau) or tau PET imaging.
- A positive (T+) result signals neurofibrillary tangle pathology.
- N (Neurodegeneration or neuronal injury):
- Identified via CSF total tau, FDG-PET hypometabolism, or MRI-detected atrophy in AD-characteristic brain regions.
- A positive (N+) result suggests active neuronal dysfunction or loss.
Individuals are scored as positive or negative for each category, resulting in biomarker profiles like A+/T+/N- or A-/T-/N+.
Why Was the A/T/N System Developed?
The framework addresses several longstanding challenges in AD research:
- Agnostic to clinical symptoms: It allows biomarker categorization independent of cognitive status, applicable across preclinical, MCI, and dementia stages.
- Clarity and simplicity: Unlike previous systems linked to diagnostic labels (e.g., "probable AD"), A/T/N focuses strictly on biological processes.
- Scalability across studies: Its binary format is useful in large-scale longitudinal and epidemiological studies, where diagnostic criteria often vary.
- Flexibility for expansion: The model supports future incorporation of additional categories, such as vascular pathology (V) or synaptic dysfunction (S), as new biomarkers emerge.
How Are A/T/N Biomarkers Measured?
Category | Biomarker Modality | Example Tests |
|---|---|---|
A | Amyloid PET, CSF Aβ42 | Pittsburgh Compound B PET, Lumbar puncture |
T | Tau PET, CSF p-tau | AV1451 PET tracer, CSF p-tau181 |
N | CSF total tau, FDG-PET, Structural MRI | CSF t-tau, parietotemporal hypometabolism, medial temporal atrophy |
Imaging biomarkers provide spatial information, while CSF biomarkers quantify disease burden but lack topographic detail. Each offers complementary insights.
Clinical Relevance and Use Cases
Individuals with A+/T+ profiles are biologically classified as having Alzheimer's disease, even if cognitively normal.
Those with A-/T+/N+ are more likely to have non-Alzheimer tauopathies, such as primary age-related tauopathy (PART).
An A-/T-/N+ profile may indicate non-AD neurodegeneration, such as cerebrovascular disease or hippocampal sclerosis.
The framework facilitates early identification, risk stratification, and clinical trial enrollment, especially as disease-modifying therapies become available for early AD.
The Role of Serum Biomarkers: A Screening Gateway
Recently, blood-based biomarkers have emerged as promising tools for enhancing accessibility to Alzheimer's disease diagnostics. These serum markers - including plasma Aβ42/40 ratios, phosphorylated tau (p-tau181, p-tau217), and neurofilament light (NfL) - offer the potential for widespread, noninvasive screening, particularly in primary care or population-based settings.
However, it is important to recognize that serum biomarkers are fundamentally screening tools, not definitive diagnostic instruments. Their primary role is to flag individuals who may benefit from further evaluation with more specific and established A/T/N modalities, such as CSF testing or PET imaging. While high-performing in recent studies, serum assays can be influenced by pre-analytical variables and have not yet fully replaced traditional measures in confirming Alzheimer's pathology.
In this context, serum biomarkers act as gateways to the A/T/N framework. They are valuable in triaging patients and guiding decisions about whether to pursue more intensive testing, but their interpretation must be cautious and aligned with clinical context. They support, rather than supplant, the core principles of biologically grounded diagnosis in Alzheimer's disease.
The A/T/N/C Model: Adding Clinical Stage
To enhance clinical utility, a fourth dimension - C (Cognition) - can be added:
- Cn = Normal cognition
- Cm = Mild cognitive impairment
- Cd = Dementia
Thus, a profile such as A+/T+/N+/Cm describes a patient with biomarker-confirmed AD and mild cognitive impairment.
Limitations and Ongoing Challenges
Biomarker cutoffs can vary by method and population, raising concerns about standardization.
Overlap with other pathologies is common, especially in older adults with mixed etiologies.
Some biomarker results may be discordant or fall near thresholds, complicating interpretation.
The framework doesn't yet fully capture individual variability, including genetic risk, resilience, or comorbid conditions.
The Path Forward
The A/T/N framework has laid the groundwork for a biologically grounded definition of Alzheimer's disease. It is now influencing regulatory standards, drug development, and real-world implementation of biomarker-supported diagnoses. Future enhancements may include:
- Integration of blood-based biomarkers (e.g., plasma Aβ42/40, p-tau217, neurofilament light).
- Addition of vascular (V) and synaptic (S) biomarkers.
- Enhanced staging models that combine molecular data with clinical phenotype and prognosis.
Conclusion
The A/T/N framework represents a transformative shift in how we define and study Alzheimer's disease. By moving beyond symptom-based diagnosis and focusing on the biology of disease, it enables earlier intervention, clearer communication, and more precise research. As diagnostic tools evolve and become more accessible, A/T/N will play a central role in the future of dementia care.